As with all inventions, it’s good to know where the technology began. Here is the often unreported origin of ultrasounds as being used for medicine.
“Pierre Curie in 1880 described the piezo electric effect whereby mechanical distortion of ceramic crystals would produce an electric charge; the reverse of this effect is used in all transducers to generate ultrasonic waves. His pupil Paul Langevin in1915 built the first hydrophone which used ultrasonic waves to locate the position and distance of submarines and is the principle behind the measurement of the fetus and abdominal masses by ultrasound. The development of Radar by Watson-Watt and his team using electro-magnetic waves in 1943 was later adapted for ultrasound to produce two dimensional images.(1)”
The first actual 2D ultrasound machine, used on pregnant women for that purpose, is credited to Ian Donald, Tom Brown (engineer), along with an engineering company. Ian Donald was using his experience with radar that he had learned while he was in the Air Force. This was of course a more primitive machine compared to ultrasound technology today (2).
https://www.ncbi.nlm.nih.gov/pmc/articl ... 9-g002.jpg
Ultrasounds for Harm?
“The modern ultrasonics era arose from Professor Langevin's 1917 invention of the quartz sandwich transducer for underwater sound transmission in submarine detection. Intense ultrasound's physical effects had not gone unnoticed in the first decade of modern ultrasonics. Langevin's tests with quartz plate transducers had resulted in killing fish in the beam of sound. Professor Van Dyke had observed in 1924 the searing of skin when a resonant quartz bar was touched, the explosive atomization of water drops from the end of the rod and friction alleviation between a metal surface and the vibrating quartz. Nevertheless, no steps were taken to investigate these early observations more fully (3).”
Wood and Loomis in 1942 created a generator of focused ultrasound and proceeded to conduct experiments with it. They were able to create focal heating in paraffin blocks, also in beef liver, without much apparent damage to the surface tissues. Animals with high intensity were able to receive temporary behavioral disabilities (such as blindness and limited mobility) via damage to the brain, however they “recovered” in 2-16 hrs; with the limited technology at the time, this wasn’t possible without damage to the surrounding tissue near the cone of radiation. They assumed this would be able to be improved with future technology.
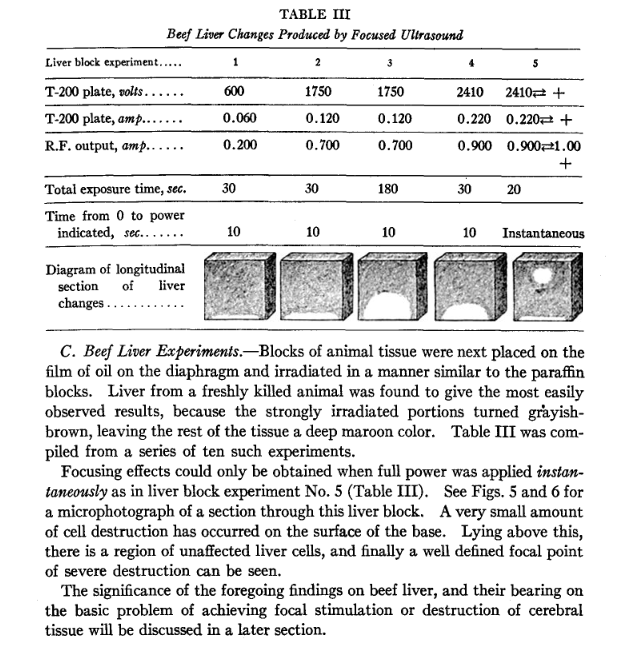 (4)
(4)Beef Liver “cooked” by focused ultrasound.
Ultrasound Risks to the Fetus
Modern Ultrasounds are safer, right?
“Ultrasound equipment manufactured before 1978 demonstrated a wide variation in ultrasonic power and intensity.18In general, ultrasound intensity was greater in equipment manufactured after 1980 than before that year,19and this increase in intensity was directly correlated with more pronounced temperature rise during use of the device.12A comparison of ultrasound output of equipment manufactured between 1995–1999 confirmed this previously identified increase in ultrasound intensities.20It appears highly likely that this trend of greater ultrasound intensity will continue, and the clinician may therefore be confronted with potential adverse effects when using newer generation ultrasound equipment. The Output Display Standard currently is the only information required by the Food and Drug Administration to alert the clinical user of the potential of an ultrasound device to produce tissue injury. The Output Display Standard purposefully overestimates such possible adverse biologic effects by assuming a reasonable “worst case” scenario. The Output Display Standard assumes linear propagation of ultrasound within a uniform, modestly attenuating tissue and describes “thermal and mechanical” indices. Acoustic power is the primary determinant of thermal and mechanical indices, but the ultrasound mode, color Doppler blood flow imaging, area of interest, transmission frequency, pulse repetition frequency, and focal zone also affect thermal and mechanical indices (5)
Heat Damage
“As much as 70% of the total temperature increase associated with ultrasound occurs within the first minute of exposure,23but temperature does continue to rise as exposure time is prolonged.24,25A linear relationship between ultrasound intensities and temperature rise has been demonstrated.24,26The relative protein content of each tissue is also an important determinant of ultrasound absorption, and hence, temperature rise. Absorption coefficients of tissues are directly related to protein content, thereby providing a surrogate marker for potential increase in tissue temperature. Absorption coefficients vary between 1 (skin, tendon, spinal cord) and 10 (bone) dB/cm MHz (table 2). The greatest temperature increase resulting from ultrasound exposure occurs in bone because of its high absorption coefficient.27Indeed, a consistent tissue temperature rise in response to ultrasound exposure has been repeatedly demonstrated in vitro , in vivo , and in utero .24,26,–,28Not surprisingly, temperature also increases in tissues adjacent to bone.23,–,25,28The absorption coefficients of fetal bone are dependent on age-related changes in mineralization, density, and heat capacity, which correlate with a faster rate of temperature increase concomitant with fetal maturity(5).”
“If there is a repetitive sequence of pulses, as in most diagnostic applications, the tissue will be warmed as a result of the absorption of acoustic energy. The temperature rise
depends on the time-averaged acoustic intensity, the acoustic absorption coefficient, the
thermal properties of tissue (heat conduction and specific heat), tissue perfusion (blood
flow), beam size and scanning mode and the period of time the transducer is held in one
position. The tissue also experiences a small transient force in the direction of propagation each time a pulse passes. If the pulse passes through a liquid, it will move in the direction of the pulse propagation: a series of pulses will cause acoustic streaming(6).”
Effects of Heating the Fetus
“Temperature fundamentally affects biochemical, physiological and reproductive processes of all living organisms. Mild increases in temperature, of less than 1 °C, may simply slightly accelerate cellular processes with no overall detrimental eff ect. Excessive temperature increase can be lethal(Raaphorst et al., 1979; Dewey et al., 1977; Dewey, 1994). Moderate temperature increases may arrest or retard cell division (Mazza et al., 2004). The effects of a moderate rise above normal physiological temperature can have important consequences for developing embryos or foetuses, particularly if the central nervous system is involved. The actively dividing cells of the embryonic and foetal central nervous system are known to be highly susceptible to changes in temperature (Edwards, 1969b; Webster and Edwards, 1984; Shiota, 1982, 1988). Interference with neural tissue is likely to have significant consequences on growth and development(6).”
Regulation? Who’s keeping us safe?
“While maximum outputs have increased, the only effective regulatory body, the Food and Drug Administration (FDA), has relaxed the upper limit on intensity that can be applied in obstetric ultrasonography in the USA. Under this new scheme (AIUM/NEMA, 1992) equipment that incorporates an output display may deliver acoustic intensity to the embryo or foetus that is almost eight times higher than equipment regulated under the Previous application-specific scheme. The rationale for this change is that the responsibility is placed on the ultrasound diagnostician to make risk/benefit assessments, based on information provided by the equipment output display, and to decide on the appropriate examination exposure conditions for each operating condition (6).”
*************************************************************************
Do you trust a random ultrasound technician not to hurt your baby with this increasingly dangerous technology?
Sources & Further Reading
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987368/
(2) https://www.ncbi.nlm.nih.gov/pmc/articl ... 8/#s3title
(3) https://www.ob-ultrasound.net/langevin.html
(4) https://www.ncbi.nlm.nih.gov/pmc/articl ... df/179.pdf
(5) https://pubs.asahq.org/anesthesiology/a ... Biological
(6) https://www.birpublications.org/pb/asse ... asound.pdf
